eCRUSADers (early career researchers using Scottish administrative data) provides a space to share information and experiences, to encourage discussion and improve the use of Scottish administrative data in research
Foreword By Dr Elizabeth Lemmon:
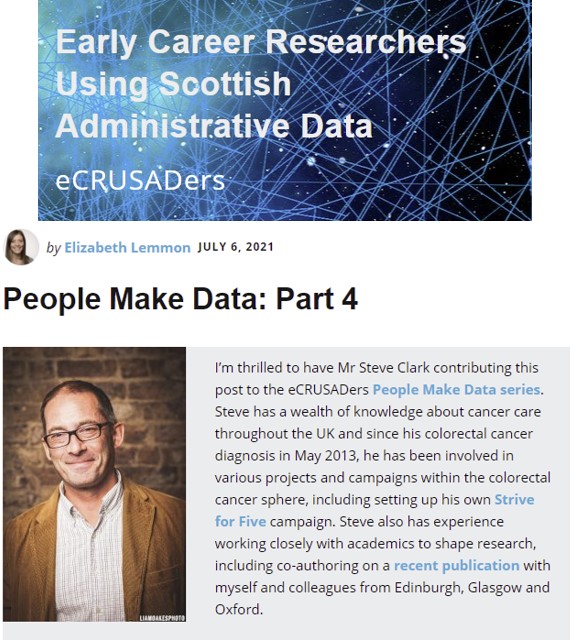
I’m thrilled to have Mr Steve Clark contributing this post to the eCRUSADers People Make Data series. Steve has a wealth of knowledge about cancer care throughout the UK and since his colorectal cancer diagnosis in May 2013, he has been involved in various projects and campaigns within the colorectal cancer sphere, including setting up his own Strive for Five campaign. Steve also has experience working closely with academics to shape research, including co-authoring on a recent publication with myself and colleagues from Edinburgh, Glasgow and Oxford.
In this post, Steve talks to eCRUSADers about his experience as a patient, his involvement in the Patient and Public Group of Bowel Cancer Intelligence UK (PPG BCI-UK) and what he has learned about the system of cancer care and cancer data during his journey. Crucially, Steve highlights the importance of actively engaging patients and the public in the research process from the outset.
Over to you Steve, the floor is yours.
I was diagnosed with advance (stage 4) colorectal cancer in May 2013, the initial prognosis looked fairly bleak as it had already spread to my liver and both lungs. I’ve been very lucky since then thanks to an excellent team who’ve given me great care – a skilled specialist colorectal surgeon was able to remove my very large primary tumour without the need for a stoma, and my chemotherapy was so successful that the planned ablation operations were cancelled. Since then I’ve been on maintenance chemo which has kept things nicely under control with only 2 recurrences in 8 years, and I’ve had clear scans for the past two years. At my recent review when I told my oncologist I was targeting 10 years he replied “and beyond”!
I’ve been aware of the fractured nature of cancer care for most of the 8 years since I was diagnosed. I’m referring here to both clinical care and patient data. I should say that I have been fortunate in my care, but through my voluntary work I’ve seen the variations evident throughout the UK.
As patients, we really need a united cancer network. A network that ensures our doctors have knowledge of, and access to, the best care for their patients. A network where the data on cancer care is available across borders to ensure best practice is readily recognised and gaps in care are addressed quickly.
As one, solitary patient, I have no way of affecting change in healthcare, but I do try to help my fellow patients as much as I can. I offer support through my Strive for Five campaign with the aim to give hope to people with a stage 4 diagnosis, but my voice is too small to affect policy. This is one of the reasons that I was keen to volunteer with some of the charities. I’m a Campaigns Ambassador with Cancer Research UK and have volunteered for some time with Bowel Cancer UK. Although most of my work with BCUK has been focussed on patient support, I’ve been involved directly with a number of key campaigns including reducing the bowel cancer screening age.
Almost two years ago I started volunteering on the Patient and Public Group of Bowel Cancer Intelligence UK (BCI-UK), my first time on a formal PPG. BCI-UK is the umbrella body overseeing two important initiatives: the UK Colorectal Cancer Intelligence Hub which runs the COloRECTal cancer Repository (CORECT-R), and the Bowel Cancer Intelligence Programme which aims to improve patient outcomes by identifying and addressing variations in care. The excellent work of the team at BCI-UK is really highlighting how vital it is that we connect the various datasets around cancer care, so that researchers can interrogate these data and directly guide improved clinical care.
The adage states the definition of madness as “doing the same thing over and over again and expecting a different result”, surely that applies to cancer care – if we don’t review what’s working best, how can we hope to improve?
And it’s not enough to simply analyse the data, the findings have to be followed up and implemented, they can be used to educate medical and surgical practitioners to help them improve their care. This could give significant improvements in patient outcomes quickly, something that is urgently needed for all patients with advanced cancer who don’t have the time to wait for new treatments to come through research – we can improve how current treatments and procedures are utilised quickly and relatively cheaply.
It’s not always about new treatments, we need better use of existing therapies through recognising and sharing best practice.
I was lucky enough to be co-author on the recent paper “Creation of the first national linked colorectal cancer dataset in Scotland: prospects for future research and a reflection on lessons learned” which is a clear step in this direction by at least making the Scottish data accessible. That’s a start, now the real work begins by making the data work for us!
Some of the ways that this type of dataset could be used for colorectal cancer care could include:
- Identifying hotspots across the country – good and bad – and addressing the gaps;
- Maintenance chemo for long term care of stage 4 – what regimens get best balance of effect and lifestyle;
- Impact of different support programmes on treatment success and tolerability;
- Clear evidence to help drive significant investment to ensure early diagnosis of cancer
I am so pleased to see more Patient and Public Groups being set up for individual studies and study groups, this can only be a good thing. I would encourage all researchers to do this as a way of ensuring their work is truly patient-centric.
This really doesn’t have to be an arduous process. The BCI-UK PPG is a large group but that’s because of the volume and range of work it’s involved in. I’m a member of other PPGs relating to individual studies that only have one or two patients, and this can work well so long as those patients can represent more than their own individual experience.
The key advice for PPG involvement is the earlier the better, ideally right at the start, when you’re at concept stage, but you can bring us in at any point. The sorts of things a PPG can help with include the more obvious things like writing the plain English version of the proposals and reviewing manuscripts, but also giving insight into what the outcomes of the study should be and what may or may not be acceptable to a patient within the study.
I truly believe that we are achieving great improvement in the care of colorectal cancer, but so much more is needed, and the way forward is by collaboration between researchers, physicians and surgeons, with patients not just at the centre of the concepts, but actively engaged.